Iron Regulation and Iron Deficiency
Learning Objectives
Describe the absorption, transport and storage of iron
Describe the role of hepcidin in the regulation of iron homeostasis
Describe the changes in haematological parameters which occur in iron deficiency
Interpret an iron panel and distinguish iron deficiency from inflammatory anaemias
Evaluation and investigation of iron deficiency
Oral iron supplementation
Iron Homeostasis
Hepcidin
is a key regulator of iron homeostasis.The action of hepcidin is to reduce (gut) enteric iron absorption
and promote sequestration (storage) in body storage compartments.
Turn off the tap (reduce bowel absorption)
Open the plug (store it away)
Hepcidin binds to the iron transport protein ferroportin,
causing the ferroprotin to be internalised and degraded by cellular lysosomes.
Ferroportin is found on enterocytes
and all organs which act as iron stores
– the liver, bone marrow and splenic macrophages.
Hepcidin levels are dependent on the rate of transcription of the hepcidin gene
transcription rates are increased in
- inflammatory states,
- when the serum iron is high
- and in iron overload.
Turn off the tap (reduce bowel absorption)
Open the plug (store it away)
Conversely, transcription rates are decreased
- in iron deficiency,
- conditions where there is increased erythropoiesis
(such as the iron-loading anaemias)
- and hypoxia.
Turn on the tap (increase bowel absorption)
stop the plug (reduce storage )
Body Iron Distribution.
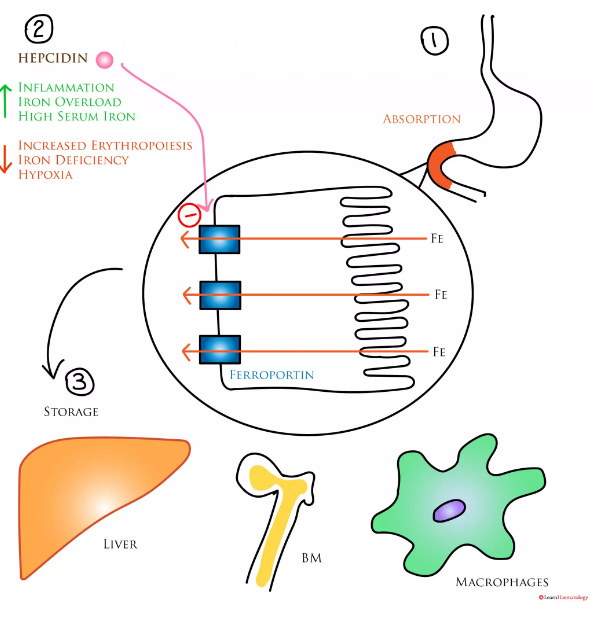
1. Iron is absorbed in the duodenum via ferroportin.
2. Hepcidin is a regulatory protein which binds to ferroportin,
causing it to be degraded by lysosomes.
Hepcidin is increased in
inflammation,
iron overload
and in the presence of high serum iron.
It is decreased in
iron deficiency,
increased erythropoiesis
and hypoxia.
3. Iron is stored in the liver, bone marrow and in splenic macrophages.
4. A significant amount also circulates as haem in haemoglobin.
Iron Homeostasis.
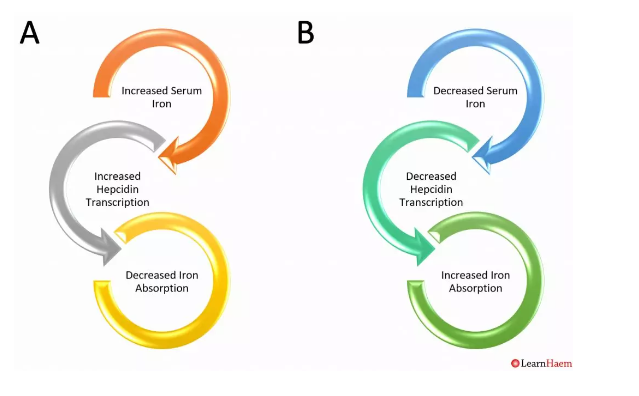
Under normal conditions, serum iron acts as a key regulator of hepcidin transcription.
Panel B: reduced serum iron levels
decrease hepcidin transcription rates,
resulting in less hepcidin binding to ferroportin
and increased enteric iron absorption.
decrease hepcidin transcription rates,
resulting in less hepcidin binding to ferroportin
and increased enteric iron absorption.
Panel A: increased levels of serum iron increase hepcidin levels,
resulting in more hepcidin binding to ferroportin
and reducing enteric iron absorption.
resulting in more hepcidin binding to ferroportin
and reducing enteric iron absorption.
IRON DEFICIENCY Clinical and Laboratory Features
Patients may present with symptoms or signs of anaemia
(fatigue, dyspnoea on exertion, chest discomfort, pallor etc.).
Alternatively, anaemia may be incidentally detected on a full blood count done for another reason.
Iron deficiency is usually characterised by a microcytic, hypochromic anaemia.
The red cell distribution width is high,
which is reflective of the anisopoikilocytosis (cells off different shapes and sizes)
which typifies iron deficiency.
the absolute red blood cell count is low,
because of the haematinic deficiency.
Thalassaemia is characterised by ineffective erythropoiesis
and decreased rates of globin chain synthesis.
Hence, the absolute red blood cell count in thalassaemia is often higher
than expected for the haemoglobin level.
(fatigue, dyspnoea on exertion, chest discomfort, pallor etc.).
Alternatively, anaemia may be incidentally detected on a full blood count done for another reason.
Iron deficiency is usually characterised by a microcytic, hypochromic anaemia.
The red cell distribution width is high,
which is reflective of the anisopoikilocytosis (cells off different shapes and sizes)
which typifies iron deficiency.
the absolute red blood cell count is low,
because of the haematinic deficiency.
Thalassaemia is characterised by ineffective erythropoiesis
and decreased rates of globin chain synthesis.
Hence, the absolute red blood cell count in thalassaemia is often higher
than expected for the haemoglobin level.
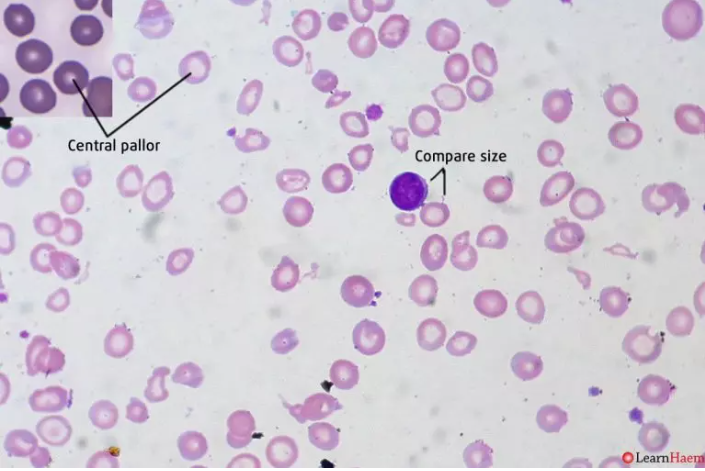
The figure below shows the blood film of a patient with iron deficiency.
This shows microcytosis, usually defined as a red cell smaller than 7µm.
As a guide, red cells should be approximately the same size as the nucleus of a normal lymphocyte.
Inset: normal red blood cells.
Note the difference in the size of central pallor, which is demonstrative of hypochroma in the iron-deficient patient
As a guide, red cells should be approximately the same size as the nucleus of a normal lymphocyte.
Inset: normal red blood cells.
Note the difference in the size of central pallor, which is demonstrative of hypochroma in the iron-deficient patient