Croup
Croup is an upper respiratory tract infection
occurring in infants and toddlers.
Parainfluenza viruses account for the majority of cases.
Rarely, other viruses are responsible, for example, RSV, influenza A and B viruses.
Unusually, it may be caused by bacteria,
for example Staphylococcus aureus.
There is a characteristic inspiratory stridor
caused by laryngeal oedema
and thick tenacious secretions
that block the trachea and airways.
The onset is slower than that of acute epiglottitis
and is usually preceded by a coryzal prodrome.
Aetiology
Croup is a generic term that covers
A heterogeneous group of diseases that affects the larynx, trachea, and bronchi (1):
Components of the croup syndrome include (1)
- laryngotracheitis
- laryngotracheobronchitis
- laryngotracheobronchopneumonitis
- spasmodic croup
Some define croup as two types
viral croup (1)
- the onset is slower and is usually preceded by a coryzal prodrome (with fever) (1)
- is an upper respiratory tract infection (acute laryngotracheobronchitis)
- affects children 6 months to 12 years of age
- has a peak incidence at two years of age
- is the commonnest cause of airway obstruction in children 6 months to 6 years of age (1)
- boys are affected more often than girls
- is commonly seen in the Autumn/fall and winter months
- parainfluenza viruses (type1, 2, 3) account for the majority of cases
- most common cause is Human parainfluenza virus 1 (HPIV-1)
- rarely, other viruses are responsible, for example
- influenza A and B viruses
- adenovirus
- measles
- RSV (Respiratory syncytial virus)
Spasmodic croup (1)
- associated with the viruses that cause viral croup
- onset is sudden, without a viral prodrome
- histology of the subglottic tissues shows noninflammatory oedema
- tends to recur
- may represent an allergic reaction to viral antigens
- often the distinction of the two types is impossible
hence sometimes spasmodic croup is considered part of the spectrum of viral croup(1)
Reference:
(1) Doug Knutson. Viral Croup. Am Fam Physician 2004;69:535-42
INFECTIOUS CROUP |
SPASMODIC CROUP |
|
Viral croup (Common) |
Bacterial croup (Rare) |
|
|
Mycoplasma pneumoniae is a rare cause of mild croup in children (1) rarely caused by Staphylococcus aureus |
|
Clinical features
Last reviewed 1 Jan 2018
Authoring team
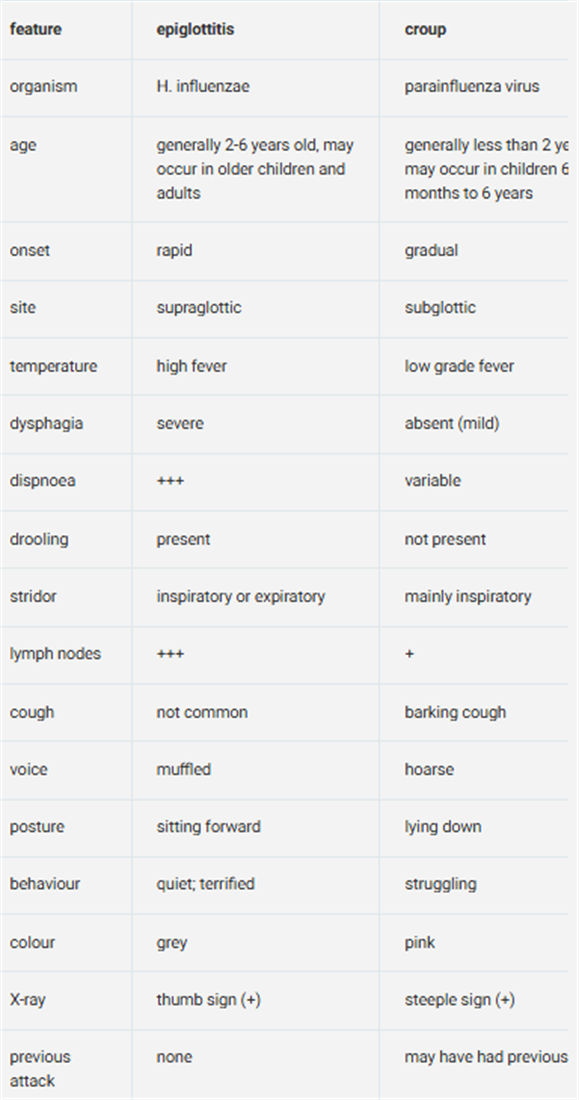
Possible clinical features include:
usually occurs in a child aged 2 years old or less;
by comparison, acute epiglottitis is normally seen in children between 2 and 6 years old
- may have a previous history of croup
- the condition is slow onset - acute epiglottitis is of fast onset
- stridor - generally inspiratory; may be biphasic
- barking cough or "croupy" cough
- no dysphagia - usually present in acute epiglottitis
- increased temperature
- child lying down - not upright as in acute epiglottitis
- the child has a hoarse voice
- dyspnoea - variable
- pink colour
- the child is struggling - not quiet as in acute epiglottitis
- symptoms worsens at night
- peak between 24 and 48 hours
- usually resolves within 7 days.
- agitation and crying aggravates symptoms
- children feel comfortable in the upright posture or when they sit up
Last reviewed 1 Jan 2018
Authoring team
Possible clinical features include:
usually occurs in a child aged 2 years old or less;
by comparison, acute epiglottitis is normally seen in children between 2 and 6 years old
- may have a previous history of croup
- the condition is slow onset - acute epiglottitis is of fast onset
- stridor - generally inspiratory; may be biphasic
- barking cough or "croupy" cough
- no dysphagia - usually present in acute epiglottitis
- increased temperature
- child lying down - not upright as in acute epiglottitis
- the child has a hoarse voice
- dyspnoea - variable
- pink colour
- the child is struggling - not quiet as in acute epiglottitis
- symptoms worsens at night
- peak between 24 and 48 hours
- usually resolves within 7 days.
- agitation and crying aggravates symptoms
- children feel comfortable in the upright posture or when they sit up
Acute epiglotitis |
Croup |
Normally seen in children between 2 and 6 years old |
Usually occurs in a child aged Up to 2 years old |
Fast onset |
Slow onset |
Child quiet |
Child struggling Agitation and crying aggravates symptoms Children feel comfortable in the upright posture or when they sit up child lying down - not upright as in acute epiglottitis
|
Dysphagia |
Dysphagia usually absent |
Investigation
investigation is probably indicated if
- a child has suffered a number of episodes of croup,
- and is especially indicated if the child was preterm
Investigations in the acute presentation may include:
Plain neck radiography (1)
The steeple sign (1)
- posterior-anterior view - shows a narrowed column of subglottic air
- lateral view -shows an overdistended hypopharynx
this sign is seen only in 50 percent of patients
Computed tomography (1)
Pulse oximetry (1)
Investigations in recurrent croup
Bronchoscopy - probably best by a paediatric chest physician
rather than an ENT surgeon
since the paediatrician will ALSO investigate below the vocal cords
Differenital diagnoses
include other causes of acute stridor such as (1):
- foreign body
- acute epiglottitis
- bacterial tracheitis
- angioneurotic oedema
- diphtheria
- peritonsillar abscess
- retropharyngeal abscess
- smoke inhalation
- burns / thermal injury
- acute laryngeal fracture
Management
Indications for hospitalization are (1):
- cyanosis
- pallor
- respiratory distress
- hypoxaemia
- stridor at rest
- toxic-looking child
- suspected epiglottitis
The management is as follows:
- Sitting the child upright may improve the croup
- Humidification using warm steam , either from a source of hot water
with care to protect the child at all times - or with an ultrasonic humidifier
however there has been no evidence of clinical benefit with this intervention in patients with moderate croup,
delivery of 100%, 40% and blow-by humidity
did not differ for change in croup scores (2)
In mild croup
(seal-like barking cough - however no stridor or sternal/intercostal recession at rest/respiratory distress)
A sytematic review has suggested that
a single dose of oral dexamethasone (0.15 mg/kg) to be taken immediately is of benefit in mild croup (3)
compared with placebo.
In most cases the child will improve within minutes.
More severe croup may require hospital admission,
although some of the following treatments may be used to buy time in the home.
If admitting a patient to hospital:
Controlled supplementary oxygen
to all children with symptoms of severe illness or impending respiratory failure
Steroid medication
Oral dexamethasone (0.15 mg/kg)
if child unable to take oral medication then
alternative possible interventions whilst awaiting admission are
- inhaled budesonide (2 mg nebulised as a single dose)
- or intramuscular dexamethasone (0.6 mg/kg as a single dose)
Steroid treatment
oral dexamethasone 0.15mg per kg,
or Oral prednisolone 1-2mg per kg,
is helpful in reducing upper airway inflammation, stridor and respiratory distress (3,4)
Nebulised steroids
there is evidence that the use of nebulised steroids reduces the need for inhaled adrenaline (4)however nebulised budesonide 2mg is more expensive than oral dexamethasone or prednisolone and no more effective
may be helpful if oral treatment is difficult.
Nebulised adrenaline
may be used at a dose of 5 ml of 1:1000 but ought to be considered as buying time with a short term benefit. At this point a child should be nursed in a high dependency area.
A transient improvement for 30-60 minutes is usually seen
Oxygen should be used with caution;
if it is required then the child is seriously ill and in danger of respiratory arrest;
its use may make the monitoring of oxygen saturations difficult
A helium-oxygen mixture has a lower viscosity and is therefore easier to breathe through a tight airway;
however it is unlikely that this will be available
no certainty of clinical benefit of this intervention (3)
Intubation and Ventilation is the final way to secure the airway
and prevent respiratory arrest in life threatening croup.
The alternative to this is
ventilation via a tracheostomy.
Notes:
Emergency management in primary care:
if a child has croup that is severe or might cause complications then the child can be given either oral prednisolone 1-2mg/kg or oral dexamethasone (2mg/5mL oral solution) 150micrograms/kg, before transfer to hospital (5)
The Cochrane review noted (4):
Glucocorticoids reduced symptoms of croup at two hours,
shortened hospital stays,
and reduced the rate of return visits to care
Uncertainty remains with regard to
the optimal type, dose, and mode of administration of glucocorticoids
for reducing croup symptoms in children
No significant difference in length of stay in the hospital or emergency department
between children treated with dexamethasone compared to budesonide,
or with dexamethasone compared to prednisolone
compared to those treated with betamethasone,
children treated with dexamethasone were at a significantly increased risk for needing epinephrine
no significant difference between children treated with dexamethasone and those treated with prednisolone
in the need for epinephrine or supplemental glucocorticoids
Reference:
(1) Doug Knutson, Viral Croup. Am Fam Physician.2004;69:535-40,541-2
(2) Scolnik D et al. Controlled delivery of high vs low humidity vs mist therapy for croup in emergency departments: a randomized controlled trial. JAMA 2006;295:1274-80.
(3) Johnson DW. Croup. BMJ Clin Evid. 2014; 2014: 0321
(4) Gates A et al. Glucocorticoids for croup in children.Cochrane Database Syst Rev. 2018 Aug 22;8:CD001955
(5) Drug and Therapeutics Bulletin 2005; 43(11):81-4.
Complications
About 15 per-cent of patients experience a complication of viral croup (1)
these include (1):
- otitis media
- dehydration
- pneumonia
- respiratory failure
Modified Westley clinical scoring system for croup
Inspiratory stridor:
Not present - 0 points
When agitated/active - 1 point
At rest - 2 points
Intercostal recession:
Mild - 1 point
Moderate - 2 points
Severe - 3 points
Air entry:
Normal - 0 points
Mildly decreased -1 point
Severely decreased - 2 points
Cyanosis:
None - 0 points
With agitation/activity - 4 points
At rest - 5 points
Level of consciousness:
Normal - 0 pointsAltered - 5 points
Total Possible Score 0-17:
<4=mild croup,
4-6=moderate croup,
>6=severe croup
Reference:
Westley CR, Cotton EK, Brooks JG; Nebulized racemic epinephrine by IPPB for the treatment of croup: a double-blind study.; Am J Dis Child. 1978 May;132(5):484-7.

