Measles
Measles is one of the most highly communicable infectious illnesses
caused by an RNA paramyxovirus,
with a morbidity and mortality underestimated by the general population.
Measles is spread by airborne or droplet transmission
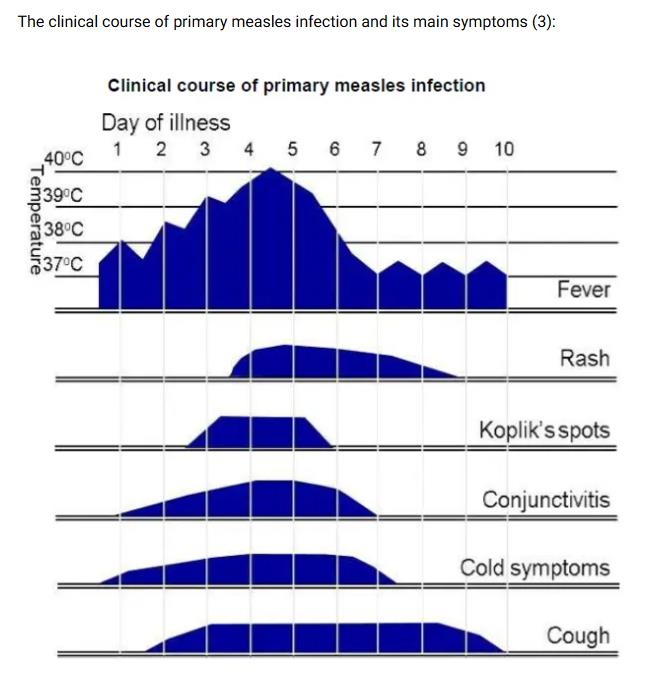
prodromal stage
Characterised by the onset of fever, malaise, coryza, coughand conjunctivitis
Koplik spots (small red spots with blueish-white centres)
may appear on the mucous membranes of the mouth
one to two days before the rash appears
and may be seen for a further one to two days afterwards
Rash is erythematous and maculopapular,
Starting at the head and spreading to the trunk and limbs over three to four days
Individuals are infectious
from the beginning of the prodromal period (when the first symptom appears)
to four days after the appearance of the rash
The incubation period is about 10 to 12 days
from exposure to onset of symptoms;
with a further two to four days before the rash appears
however..
the incubation period can vary from 7 to 21 days (3)
If a child has the following features then these are strongly suggestive of measles:
- rash for at least three days, and
- fever for at least one day, and
- at least one of the following - cough, coryza or conjunctivitis
It is severe in infants, adults and immunocompromised patients (2).
Measles is a notifiable disease in the UK (since 1940).
Notification can be done on clinical suspicion (laboratory confirmation not needed) (1).
What Is Measles?
Kristin Walter, MD, MS1; Preeti N. Malani, MD, MSJ2
Measles (rubeola) is an infection
caused by a highly contagious virus primarily spread by respiratory droplets.
How Common Is Measles and How Contagious Is It?
Measles is currently rare in the US because highly effective vaccines are given as part of routine childhood immunizations.
Over the past 2 decades, sporadic outbreaks of measles have occurred in the US,
ranging from 37 cases in 2004
to 1282 in 2019.
Measles outbreaks in the US
often originate from an individual who becomes infected while in another country
and then spreads the virus to unvaccinated individuals in the US.
Measles is one of the most contagious infections to affect humans.
The virus is spread through airborne droplets
or by direct inoculation through the nose, mouth, or eyes after touching an infected surface.
People with measles can spread the virus
starting about 4 days before the onset of rash
through 4 days after their rash appears.
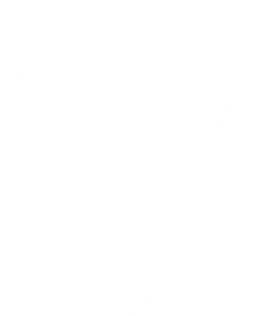
What Are the Common Signs and Symptoms of Measles?
Common symptoms of measles are fever, cough, runny nose, red and watery eyes (conjunctivitis),
and rash. Small white spots typically appear on the inside of the cheek 2 to 3 days before the rash starts.
The measles rash consists of flat red spots that spread from the head to the lower extremities.
What Are Potential Complications and Who Is at Risk?
Measles can lead to
- pneumonia,
- ear infections
- upper airway infection,
- pain and sores in the mouth,
- and diarrhea.
Rare but serious neurologic complications include
- swelling of the brain and spinal cord
- or progressive neurologic disorders
that develop weeks to years after measles infection.
Approximately 1 to 3 per 1000 people infected with measles
die from respiratory or neurologic complications.
People at highest risk of developing complications from measles include
- unvaccinated individuals younger than 5 years or older than 20 years
- and those who are immunocompromised
- or pregnant.
Measles acquired during pregnancy can result in preterm labor and low infant birth weight.
How Is Measles Diagnosed?
Measles is most commonly diagnosed by identifying the virus
in throat or nasopharyngeal swabs, saliva, or urine
using a laboratory test that identifies genetic material in a sample (RT-PCR).
How Can Measles Be Prevented?
Vaccination is safe and highly protective against measles.
The CDC recommends that all children receive 2 doses of the measles-mumps-rubella (MMR) vaccine:
the first dose at 12 to 15 months
and the second at 4 to 6 years.
The measles, mumps, rubella, and varicella (MMRV) vaccine
also protects against measles and can be given to children aged 12 months to 12 years.
College and university students without prior measles vaccination or infection
should receive 2 doses of MMR vaccine,
spaced at least 28 days apart.
Adults born in 1957 or later without evidence of immunity against measles
should be given at least 1 dose of MMR vaccine.
How Are Patients and People Exposed to Measles Treated?
There are no proven effective antiviral treatments for measles.
Infected individuals should be isolated
and monitored closely for complications.
The CDC recommends vitamin A supplementation for children hospitalized with measles.
People without previous measles vaccination or infection
should receive the MMR vaccine within 72 hours or immunoglobulin
(derived from donated blood that contains antibodies to measles)
within 6 days of exposure to a patient with measles.
though transmission route of measles is mostly airborne by droplet spread or direct contact with nasal or throat secretions of infected persons; much less commonly, measles may be transmitted by articles freshly soiled with nose and throat secretions, or through airborne transmission with no known face-to-face contact (3)
measles is extremely infectious, with a basic reproduction number (R0) estimated around 15 to 20 (that is, on average, there will be 15 to 20 individuals infected from a single case in a totally susceptible population) (3)
the secondary attack rate is highest among close unimmunised contacts, particularly household contacts
Reference:
(1) Immunisation Against Infectious Disease - "The Green Book".Chapter 21 Measles (August 2019)
(2) Asaria P, MacMahon E. Measles in the United Kingdom: can we eradicate it by 2010? BMJ. 2006;333(7574):890–895
(3) UK Health Security Agency (February 2024). National measles guidelines
(4) NHS England (January 19th 2024). Guidance for risk assessment and infection prevention and control measures for measles in healthcare settings.
measles is extremely infectious, with a basic reproduction number (R0) estimated around 15 to 20 (that is, on average, there will be 15 to 20 individuals infected from a single case in a totally susceptible population) (3)
the secondary attack rate is highest among close unimmunised contacts, particularly household contacts
Reference:
(1) Immunisation Against Infectious Disease - "The Green Book".Chapter 21 Measles (August 2019)
(2) Asaria P, MacMahon E. Measles in the United Kingdom: can we eradicate it by 2010? BMJ. 2006;333(7574):890–895
(3) UK Health Security Agency (February 2024). National measles guidelines
(4) NHS England (January 19th 2024). Guidance for risk assessment and infection prevention and control measures for measles in healthcare settings.
Epidemiology
During the pre vaccine era around 100 deaths were seen annually in the UK
but since the introduction of MMR vaccine in 1988
the disease has become relatively rare (1)
(only one death from acute measles in a 13 year old child have been reported since 1992) (2).
Recently an increase in measles cases has been reported in UK
with the first mortality reported (in 2006) since 1992 (1).
This has been due to a failure of uptake of vaccination over the past decade (3).
Mortality due to measles is age related
mortality is highest in children under one year
and lowest in children aged between 1 to 9 years
again the it rises with advancing age (2)
Globally there were 164 000 measles deaths out of which 95% occurred in low-income countries (4)
Reference:
1. Asaria P, MacMahon E. Measles in the United Kingdom: can we eradicate it by 2010? BMJ. 2006;333(7574):890-895
2. Health Protection Agency (HPA). Background Information on Measles
3. Health Protection Agency (HPA) 2008. Measles figures soar
4. World Health Organization (WHO). Measles
Clinical features
After an incubation period of around ten days (range 7 to 18 days) (1),
clinical features develop as follows:
Catarrhal stage:
prodromal illness (lasts 2-4 days) with fever, coryza, conjunctivitis, and cough
Koplik spots -
pathognomonic for measles
bright red spots with a bluish white speck at the centre is seen on the buccal mucosa, especially on the inside of the cheeks
usually appears just before the onset of rash and continue for 2 or 3 days (3)
sometimes generalised lymphadenopathy
irritability
infective from onset
photophobia
sore throat
abdominal pain (3)
Exanthematous stage:
rash appears 3 to 5 days later, maculopapular, firstly behind the ears,spreads to the face, then down the body, becoming confluent, fading by the third day
severity of other symptoms may increase 2 – 4 days before the onset of the rash with the symptoms being most severe on the first day of rash (3)
Clinical recovery in uncomplicated measles may be seen shortly after the emergence of the rash (2).
In immunocompromised patients fever or rash may not be present for weeks or months after exposure (2).
Treatment
The disease is usually self limiting in immunocompetent people (1).
Important to be aware of the possible complications
- isolation
- analgesics for headache and backache
- treatment of bacterial superinfection
- monitor and correct nutritional and hydrational changes; measles may produce dramatic weight reduction
prognosis generally very good in the developed world
in the developing world measles is a major cause of morbidity and mortality:
up to 40% mortality in some studies;
dependent upon the nutritional status of the sufferer.
Younger children are affected in the developing world
compared to the developed world.
measles is a notifiable disease in the UK
Management of contacts:
non-vaccinated contacts (over the age of 9 months) of the sufferer should be given live measles vaccine,
best within 3 days of the exposure (1),
but up to 6 days in particular patients such as immunocompromised
in case of MMR being too late to provide effective post-exposure prophylaxis,
it will offer protection against future exposure in previously unvaccinated individuals (2)
may be given intravenous immunoglobulin
as soon as possible after exposure(ideally within 6 days) (2)
alternatively, immunodeficient contacts,
pregnant women negative for measles IgG
or those under the age of nine months
The disease is infectious for four days after the onset of the rash (1).
Reference:
(1) Asaria P, MacMahon E. Measles in the United Kingdom: can we eradicate it by 2010? BMJ. 2006;333(7574):890–895
(2) Immunisation Against Infectious Disease - "The Green Book".Chapter 21 Measles (August 2006)
Complications
Most common:
otitis media (7-9%)
bronchopneumonia, often with Staphylococcus aureus or gram-negative organisms in undernourished children (1-6 %)
diarrhoea (8%)
febrile convulsions (1 in 200) (1)
Less common:
meningitis
immunosuppression, with giant cell pneumonitis in the immune suppressed
gastric symptoms
Rare:
encephalitis - which develops 7-10 days after the onset of symptoms
late complication of bronchiectasis
Very rare:
subacute sclerosing panencephalitis
affects 1 in 25 000 cases, but the risk of getting SSPE is 16 times higher in children who develop measles under 1 year of age when compared to those infected over 5 years (1)
SSPE occurs around seven years after the onset of symptoms but may occur after two or three decades (1).
Measles during pregnancy may lead to potentially fatal pneumonitis in mother, an increased risk of spontaneous abortion, premature delivery, and low birth weight babies. No congenital abnormalities have been found in babies born to mothers who contracted measles during pregnancy (2).
Note that tuberculosis is more common in children following measles. This is related to a depression in cell-mediated immunity and lymphopaenia.
Complications are more common and more severe in poorly nourished and/or chronically ill children, including those who are immunosuppressed (upto 80%)
in patients with cancer - case fatality rate is around 70%
in HIV infected patients - case fatality rate is between 5-40% (2)
Reference
(1) Immunisation Against Infectious Disease - "The Green Book".Chapter 21 Measles (August 2006)
(2) Asaria P, MacMahon E. Measles in the United Kingdom: can we eradicate it by 2010? BMJ. 2006;333(7574):890–895
Prophylaxis
Every susceptible person (regardless of age) must be protected from measles. Protection against mumps or rubella should also be considered in these patients (1).
there is no upper age limit for vaccination
viruses in vaccines are never transmitted and do not pose a threat to susceptible contacts
immunocompromised people should be protected from being exposed to measles
and if necessary any unprotected household contacts
or other close contacts should be immunized (1)
Prophylaxis is with the use of live vaccine,
and with the use of immunoglobulin in some contacts.
Reference
(1) Asaria P, MacMahon E. Measles in the United Kingdom: can we eradicate it by 2010? BMJ. 2006;333(7574):890–895
Measles in pregnancy
there is no evidence to support an association between measles in pregnancy and congenital defects (1)
however, the need for effective post-exposure protection
is supported by studies suggesting a high risk of
severe maternal morbidity,
fetal loss
and prematurity
measles is more severe in pregnancy,
and increases the risk of
miscarriage, stillbirth, or preterm delivery (2)
measles in late pregnancy can also lead to perinatal infection in the infant,
which may be associated with a high mortality
and the risk of subacute sclerosing panencephalitis
UK guidance recommends using human normal immunoglobulin
for susceptible pregnant women exposed to measles (1,2)
although there is no direct evidence
that this will reduce the complications of measles in pregnancy,
it may attenuate disease
and therefore reduce the rate of complications
measures to identify women likely to be susceptible include
assessment of age,
vaccination history,
and/or antibody testing
main aim of measles PEP (post exposure prophylaxis) for pregnant women
is attenuation of disease
and therefore human normal immunoglobulin (HNIG) can be used (2)
will be issued up to 6 days after exposure,
allowing time for assessment of immunity status in most instances (2)
where a second exposure occurs more than 3 weeks after a first dose of immunoglobulin,
a further dose may need to be considered (2)
Post exposure prophylaxis (PEP) with human normal immunoglobulin
is recommended for neonates with recent in utero exposure,
that is those born to mothers
who develop a measles rash 6 days before to 6 days after delivery (2):
Pregnant women do not require post-exposure prophylaxis
if they are inadvertently given MMR (2)
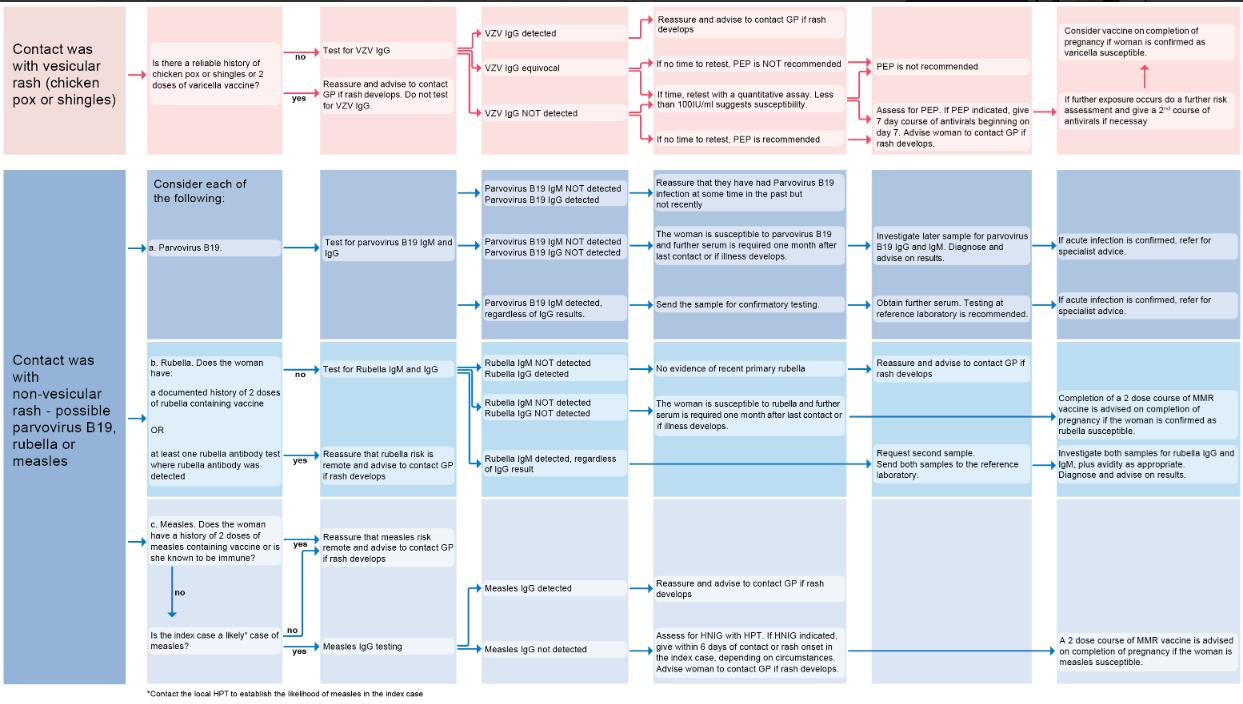
If considering an infectious cause for the development of the rash in pregnancy.
A flowchart summarising contact with vesicular or non-vesicular rash (3):
Open Image in Modal
Reference:
1) Manikkavasagan G, Ramsay M.The rationale for the use of measles post-exposure prophylaxis in pregnant women: a review. J Obstet Gynaecol. 2009 Oct;29(7):572-5.
2) UK Health Security Agency (July 2024). National measles guidelines
3) UK Health Security Agency (July 2024). Guidance on the investigation, diagnosis and management of viral illness (plus syphilis), or exposure to viral rash illness, in pregnancy
Breakthrough measles
Breakthrough measles (reinfection)
The term 'breakthrough measles' (previously referred to as 'reinfection')
is used to describe a confirmed case of measles
in someone who developed immunity to measles,
either from natural measles
or from prior receipt of measles containing vaccine.
cases of breakthrough measles are generally mild,
have a shorter duration
and may not have the full triad of cough, coryza and conjunctivitis
in some cases of breakthrough measles
a typical rash may not be observed.
The immunological characteristics of breakthrough measles
differ from those of primary vaccine failure,
which is thought to occur when patients never develop immunity,
for example when measles vaccine is given in the presence of maternal antibody
in contrast, breakthrough measles cases are thought to arise
when antibody levels from past immunity wane,
usually after many years,
and subsequent close exposure
can lead to measles viral replication
and a consistent illness.
Breakthrough measles cases are usually seen in patients
who have received 2 doses of measles-containing vaccine,
and antibody testing may be misinterpreted
infectivity of these cases is lower
than in primary measles infection,
and transmission from breakthrough measles is rare,
probably due to low and transient infectivity
for this reason, tracing the contacts of presumed breakthrough measles
can be limited to those at highest risk of complications
and/or with a very high level of exposure.
In measles endemic areas breakthrough cases represent fewer than 10% of total infections,
but this will increase as vaccination coverage in the general population rises (2)
In a highly vaccinated population
and with the increasing availability of PCR testing
it is inevitable that more breakthrough measles infections will be identified
for example it is not unusual to pick up breakthrough infections in outbreaks
linked to healthcare or other settings through active case finding
it is important to note that breakthrough measles
is not thought to pose a significant public health threat
in the context of global measles elimination efforts
Reference:
Public Health England (November 2019). National measles guidelines.
UK Health Security Agency (February 2024). National measles guidelines