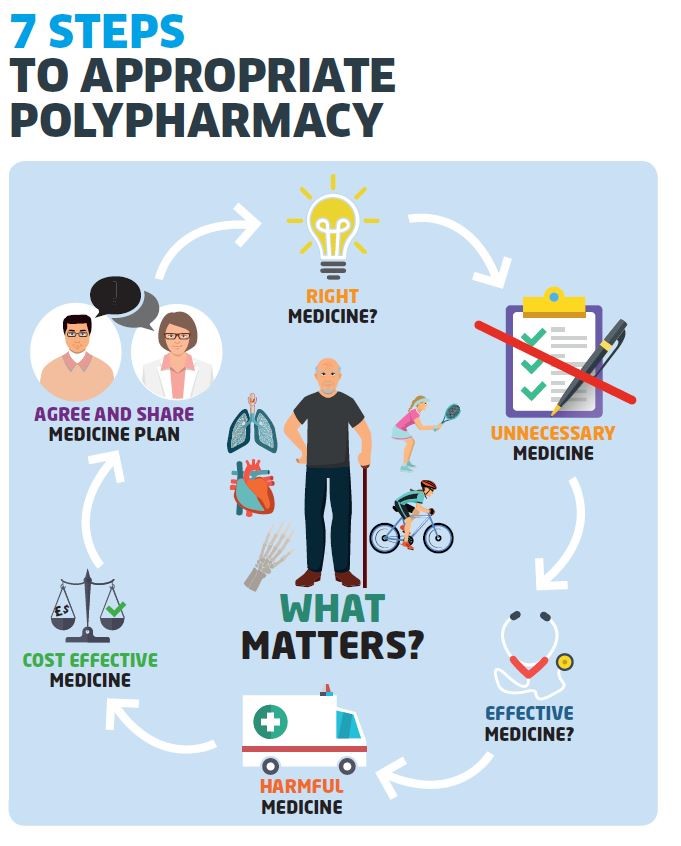
The following 7-Steps are intended as a guide
to structure the review process and are presented as:
N.B. No list can be comprehensive and the reviewers clinical judgement and experience continues to
be essential in tailoring the advice given to the needs of an individual patient and to identify other
additional medication related problems.
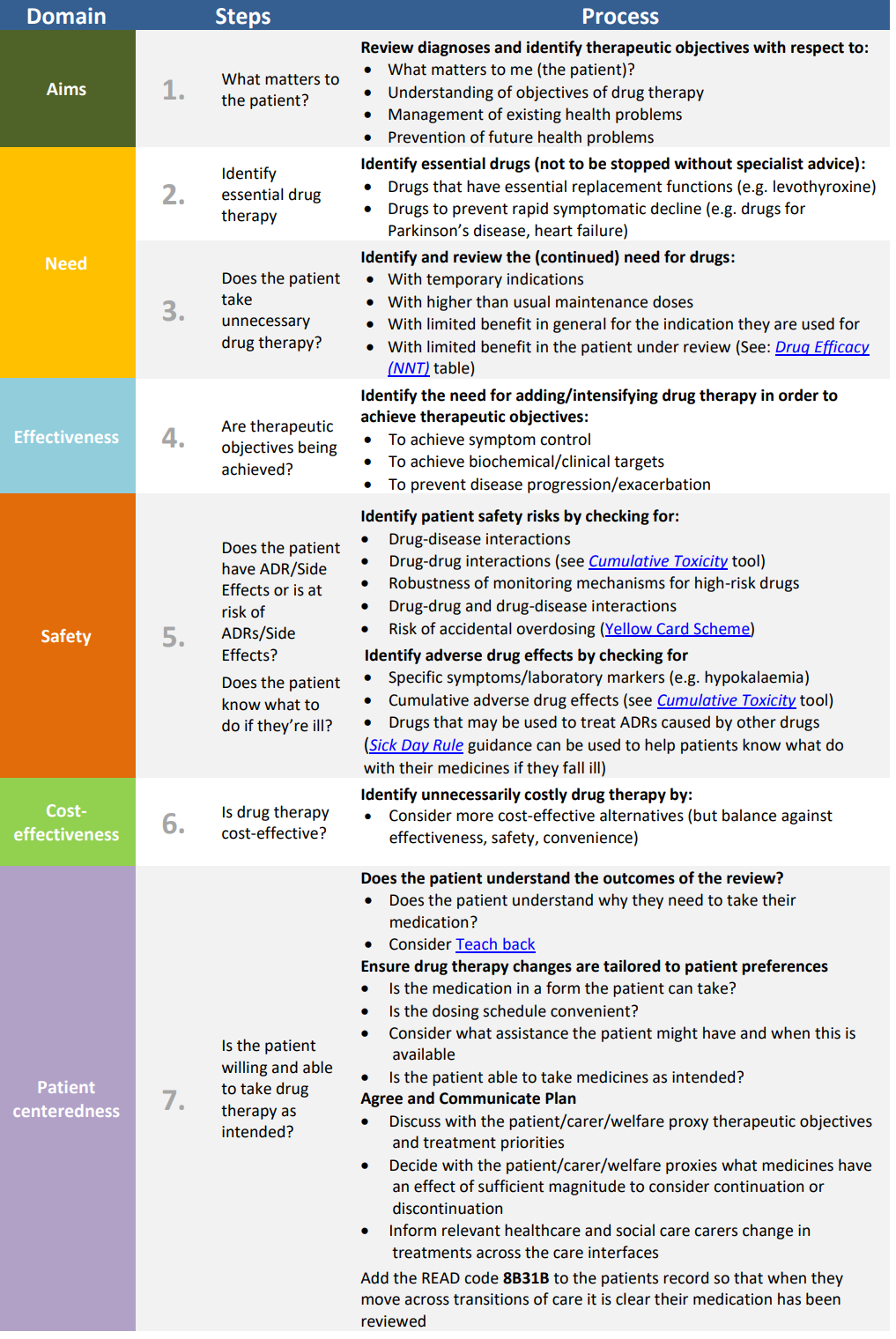
Step 1: (Aim) What matters to the patient?
· Identify aims and objectives of drug therapy by asking the patient what matters to you?
· Explain any key information such as laboratory markers
· Establish treatment objectives with the patient through shared decision making
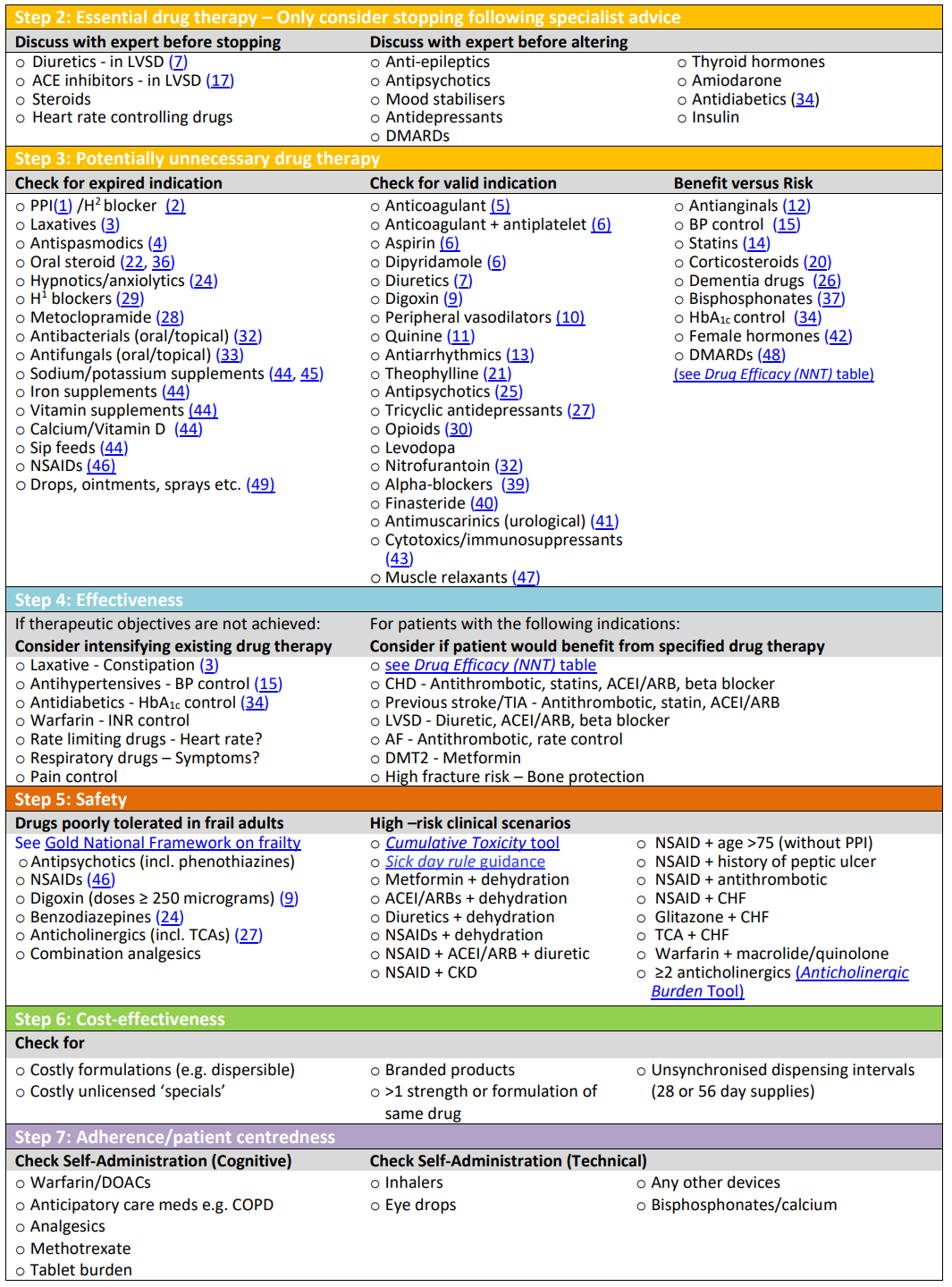
Step 2: (Need) Identify essential drug therapy.
· Separate the list of medicines which the patient is taking
· Ensure the patient understands the importance of essential drug therapy
· All medication whether herbal, prescribed or traditional remedies should be included
Step 3: (Need) Does the patient take unnecessary drug therapy?
· For the remaining drugs, it should be verified that each has a function in achieving the
therapeutic goals or outcomes that matter most to the patient
· Review preventative treatment to ensure the patient is able to continue taking medicine for
required time to gain benefit (Drug Efficacy (NNT) table).
· Can lifestyle changes replace any unnecessary drug therapy?
Step 4: (Effectiveness) Are therapeutic objectives being achieved?
· Check treatment choice is the most effective to achieve intended outcomes
· If this is not the case, the possibility of patient non-adherence should be investigated as a
potential explanation. Otherwise, the need for dose titration may also be considered. 50% of
patients taking four or more medicines don’t take them as prescribed (Medication Adherence:
WHO Cares?).
Step 5: (Safety) Is the patient at risk of ADRs or suffers actual ADRs?
· The presence of ADRs can sometimes be identified from laboratory data (e.g. hypokalaemia
from diuretic use)
· The patient may report such symptoms (including drug-drug and drug-disease interactions, but
also the patient’s ability to self-medicate)
· Ask the patient specific questions (e.g. about the presence of anticholinergic symptoms,
dizziness or drowsiness). If patient is experiencing ADRs, use Yellow Card Reporting
Step 6: (Efficiency) Is drug therapy cost-effective?
· Opportunities for cost minimisation should be explored, but changing drugs for cost reasons
should only be considered if effectiveness, safety or adherence would not be comprised
· Ensure prescribing is in line with current formulary recommendations
Step 7: (Patient-centred) Is the patient willing and able
to take drug therapy as intended?
· Does the patient understand the outcome of the review?
· Ensure drug therapy is tailored to patient preferences
· Agree and communicate plan with patient and/or welfare proxy
· Even if adult lacks capacity, adults with Incapacity Act still requires that the adult’s views are
sought. Ensure “Adults with Incapacity Documentation” in place
to structure the review process and are presented as:
N.B. No list can be comprehensive and the reviewers clinical judgement and experience continues to
be essential in tailoring the advice given to the needs of an individual patient and to identify other
additional medication related problems.
Step 1: (Aim) What matters to the patient?
· Identify aims and objectives of drug therapy by asking the patient what matters to you?
· Explain any key information such as laboratory markers
· Establish treatment objectives with the patient through shared decision making
Step 2: (Need) Identify essential drug therapy.
· Separate the list of medicines which the patient is taking
· Ensure the patient understands the importance of essential drug therapy
· All medication whether herbal, prescribed or traditional remedies should be included
Step 3: (Need) Does the patient take unnecessary drug therapy?
· For the remaining drugs, it should be verified that each has a function in achieving the
therapeutic goals or outcomes that matter most to the patient
· Review preventative treatment to ensure the patient is able to continue taking medicine for
required time to gain benefit (Drug Efficacy (NNT) table).
· Can lifestyle changes replace any unnecessary drug therapy?
Step 4: (Effectiveness) Are therapeutic objectives being achieved?
· Check treatment choice is the most effective to achieve intended outcomes
· If this is not the case, the possibility of patient non-adherence should be investigated as a
potential explanation. Otherwise, the need for dose titration may also be considered. 50% of
patients taking four or more medicines don’t take them as prescribed (Medication Adherence:
WHO Cares?).
Step 5: (Safety) Is the patient at risk of ADRs or suffers actual ADRs?
· The presence of ADRs can sometimes be identified from laboratory data (e.g. hypokalaemia
from diuretic use)
· The patient may report such symptoms (including drug-drug and drug-disease interactions, but
also the patient’s ability to self-medicate)
· Ask the patient specific questions (e.g. about the presence of anticholinergic symptoms,
dizziness or drowsiness). If patient is experiencing ADRs, use Yellow Card Reporting
Step 6: (Efficiency) Is drug therapy cost-effective?
· Opportunities for cost minimisation should be explored, but changing drugs for cost reasons
should only be considered if effectiveness, safety or adherence would not be comprised
· Ensure prescribing is in line with current formulary recommendations
Step 7: (Patient-centred) Is the patient willing and able
to take drug therapy as intended?
· Does the patient understand the outcome of the review?
· Ensure drug therapy is tailored to patient preferences
· Agree and communicate plan with patient and/or welfare proxy
· Even if adult lacks capacity, adults with Incapacity Act still requires that the adult’s views are
sought. Ensure “Adults with Incapacity Documentation” in place
MEDICATION REVIEWS AND CONDITIONS
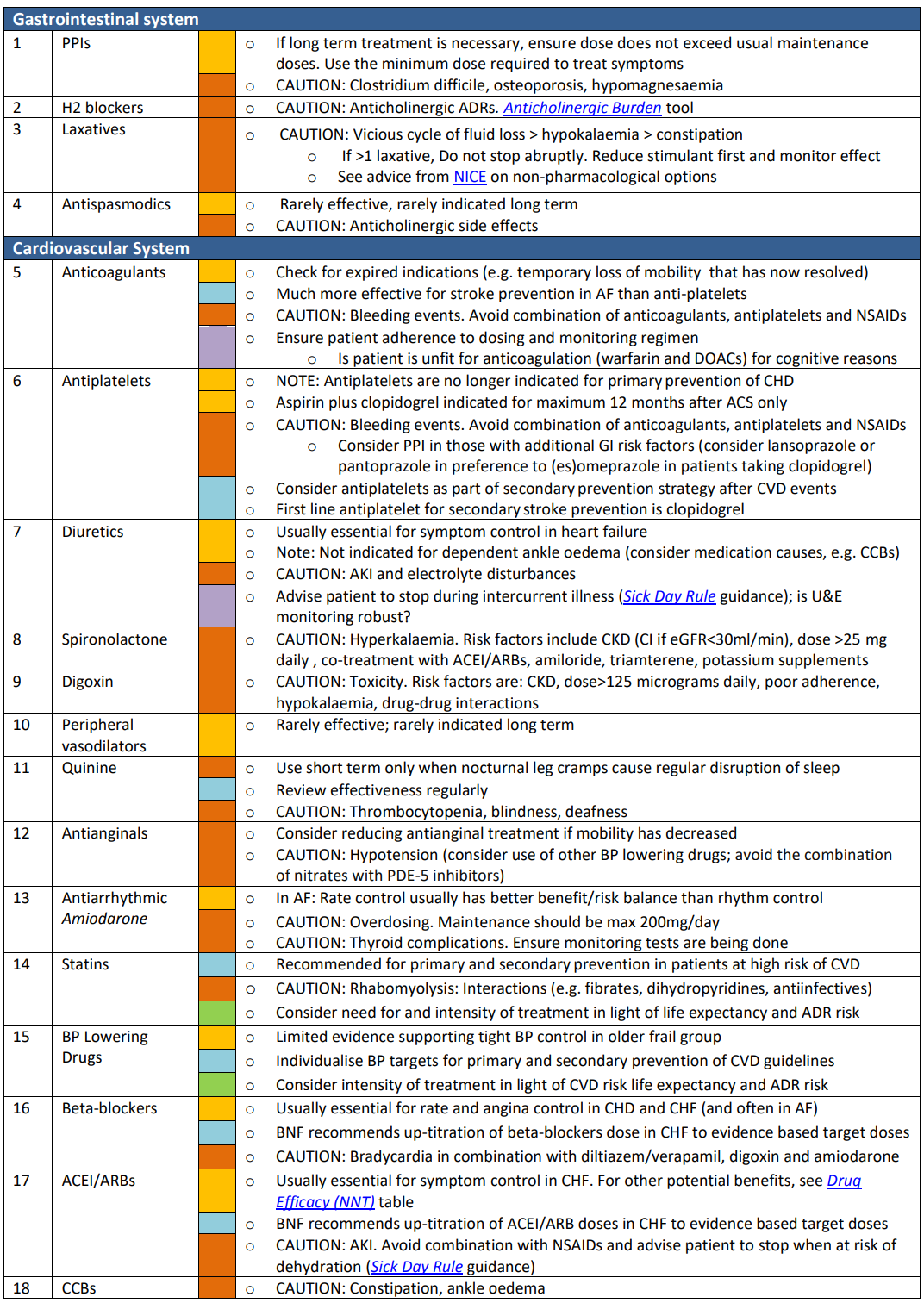


.png)