Thyroid abscess
Infection of the thyroid is rare.
usually occurs in young children or debilitated patients.
Most often, it occurs secondary to infection elsewhere.
Bacterial infection is most common.
Agents include staphylococcal aureus - in one third of cases -
streptococci, Salmonella, Enterobacter and mycobacteria.
Fungal infection is rare.
Presentation is usually with painful enlargement of the thyroid gland.
The condition is usually transient.
It may be treated with surgical drainage and antibiotics.
Long term thyroid dysfunction is rare.
Thyroiditis
The most common and well characterised forms of thyroiditis are:
- Hashimoto's thyroiditis (or Autoimmune thyroiditis)
- Subacute granulomatous thyroiditis (or De Quervains)
- Subacute lymphocytic thyroiditis (Painless thyroiditis)
- Riedel's thyroiditis
Less common and less characterised forms are:
- Acute or Infective thyroiditis
- Infiltrative thyroiditis
e.g. sarcoidosis, tuberculosis
Thyroid function tests
The laboratory assessment of hypo- and hyperthyroidism
has been simplified by the development of sensitive assays for:
TSH
Free T3 / Free T4
Some laboratories still measure
Total T3 and Total T4
Thyroid binding protein concentrations
must be known to interpret total levels
Some typical reference ranges in adults are:
Note that reference ranges may vary between laboratories.
TSH - 0.4 – 4.5 mU/L
FT3 - 3.5 – 7.8 nmol/L
FT4 - 9.0 – 25 pmol/L
TT3 - 1.2 – 2.6 nmol/L
TT4 - 60 – 160 nmol/L
NICE state: BIOTIN
ask adults, children and young people with suspected thyroid dysfunction
about their biotin intake
A high consumption of biotin from dietary supplements may lead to falsely high or low test results
Reference:
(1) Association for Clinical Biochemistry (ACB), British Thyroid Association (BTA), British Thyroid Foundation (BTF) 2006. UK guidelines for the use of thyroid function tests
(2) NICE (October 2023). Thyroid disease: assessment and management
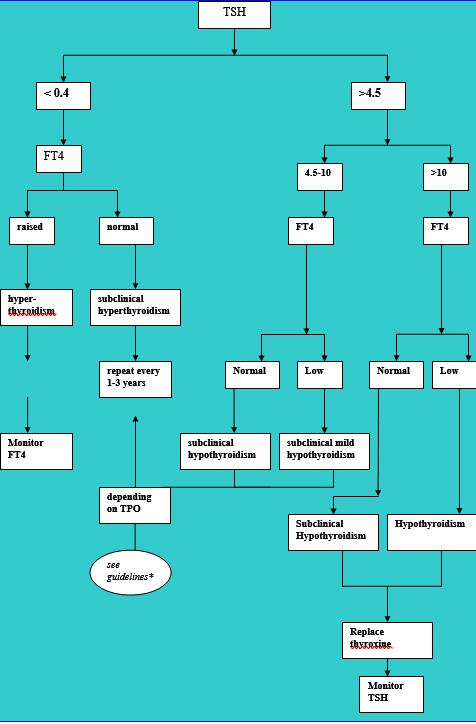
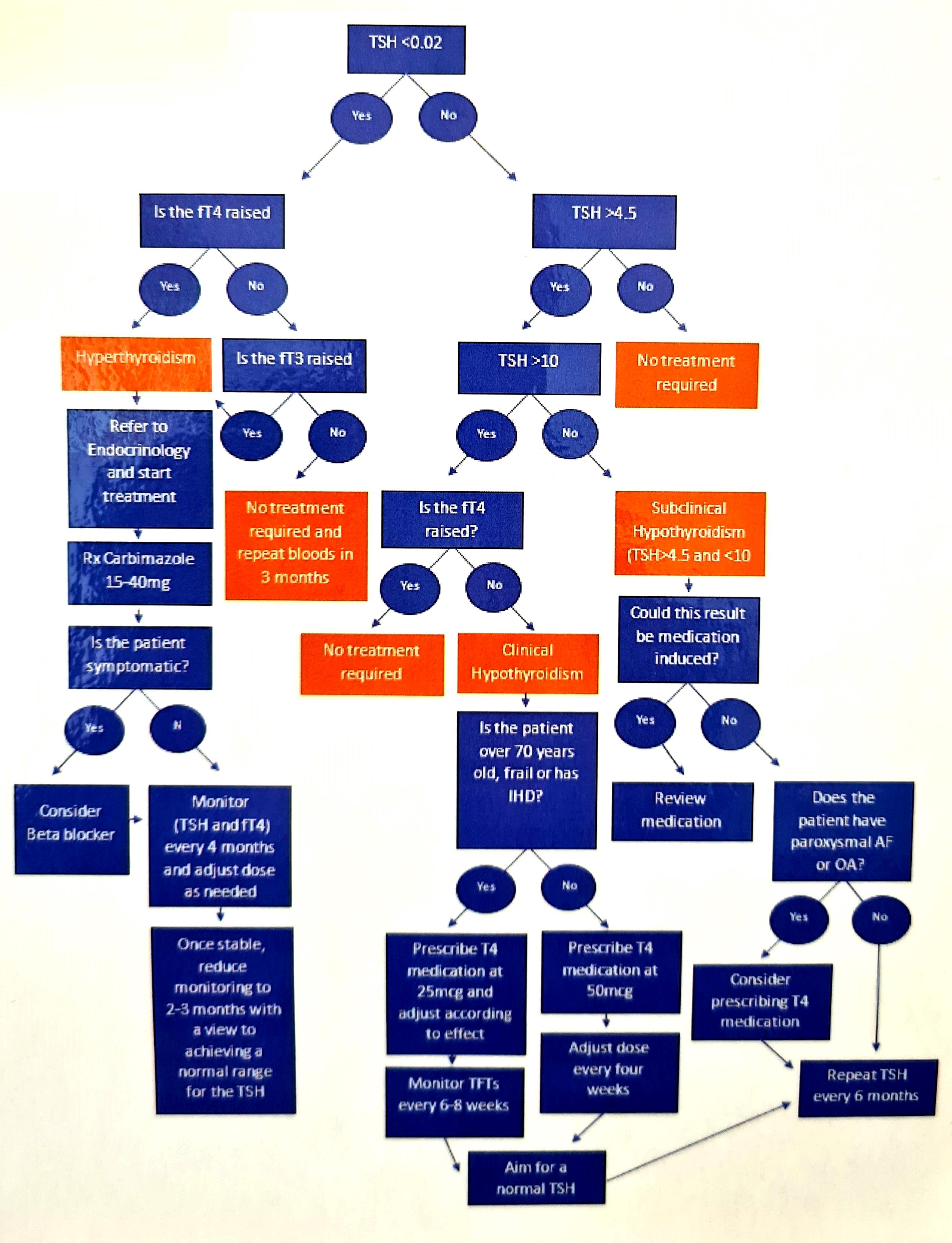
Thyroid disease diagnostic algorithm
Where TSH and free T3 or T4 are measured as the first-line thyroid investigation
there are six patterns of abnormality:
TSH may be high or low
free T3 or free T4 may be
low, normal or high
Reference:
Dayan CM. Interpretation of thyroid function tests. Lancet 2001;357:619-24.
|
TSH Low |
TSH High |
FT3/FT4 Low |
|
|
FT3/FT4 Normal |
|
|
FT3/FT4 High |
|
|
Low TSH, Raised free thyroid hormones
A depressed TSH with elevated free T3 or T4 is characteristic of
Primary hyperthyroidism.
In most cases the radioiodine thyroid scan will show increased signal.
The 3 common causes of primary hyperthyroidism are:
- Grave's disease:
Antithyroid antibodies in 90% of cases
radioiodine scan: diffuse uptake
- Multinodular goitre
- Toxic nodule
Other diagnoses to consider are:
- Transient thyroiditis:
subacute, silent or post-partum
usually a short history
rapid return to euthyroidism with treatment
- De Quervain's thyroiditis:
A tender thyroid
Raised ESR
Low TSH, Normal free thyroid hormones
The most common cause of these test results is
Excessive thyroxine ingestion.
Otherwise the combination of a suppressed TSH and normal free thyroid hormones
is usually an asymptomatic disorder termed
Subclinical hyperthyroidism.
Subclinical hyperthyroidism, In the elderly, is often caused by multinodular goitre.
Rare causes of low TSH with normal free thyroid hormones are seen in hospital practice:
- high dose steroid therapy
- dopamine infusion
- dobutamine infusion
- other systemic illness
Complete suppression of TSH (<0.1 mU/L)
merits treatment for hyperthyroidism
because of the significant increased morbidity associated with subclinical hyperthyroidism
Low or normal TSH, Low free thyroid hormones
This combination is most frequently seen in patients with other non-thyroid illness.
In the patient who is not systemically unwell then
the low TSH may reflect
Pituitary pathology
with secondary hypothyroidism.
It is important to make this diagnosis because:
the associated hypoadrenalism may be fatal
pituitary tumours may cause severe local damage
The investigation should include:
Short Synacthen test
FSH, LH and sex steroid determinations
MRI of the brain
Patients who have recently been treated for hyperthyroidism
may have residual suppression of TSH levels for up to a year.
Such patients who have low TSH and low free thyroid hormones
are hypothyroid and should be treated as such.
Raised TSH, low free thyroid hormones
Raised TSH in combination with low free thyroid hormones is caused by
Primary hypothyroidism.
Raised TSH, Normal free thyroid hormones
The large majority of patient with raised TSH and normal free thyroid hormones are suffering from
Subclinical autoimmune hypothyroidism.
These results occur more rarely in the following circumstances:
- The presence of heterophile antibodies
Mouse antibodies are used in many TSH assays
patients may have antibodies to mouse immunoglobulins
heterphile antibodies result in a false TSH elevation
Alternative assays should be used for these patients
- Thyroxine malabsorption
in patients taking a regular dose of thyroxine
an increase in the TSH concentration
may indicate thyroxine malabsorption, due to:
small bowel disease
cholestyramine
iron therapy
- Amiodarone therapy
- Recovery from severe non-thyroidal disease
- Congenital abnormalities of thyroid function:
some cases of Pendred's syndrome
Normal or raised TSH, raised free thyroid hormones
Normal or elevated TSH in the presence of raised free thyroid hormones
is a rare disorder but may be clinically important.
The causes of this pattern of abnormality are:
- Artefact - need to repeat the tests
- Interfering antibodies
- Familial dysalbuminaemic hyperthyroxinaemia
- amiodarone therapy
- thyroid hormone receptor mutations
- acute psychiatric disease
- TSH secreting pituitary tumour
- Intermittent thyroxine overdosage
More specialist tests of thyroid function include:
TRH test
thyroid scanning
thyroid ultrasound
thyroid antibodies
Thyroid autoantibodies
1. Thyroglobulin autoantibodies
are present in:
- Grave's disease
- Hashimoto's thyroiditis
- Idiopathic thyroid atrophy
- De Quervain's thyroiditis - transiently
- Without thyroid disease in 7% of males, and 15-20% of females
2. Anti thyroid peroxidase antibodies
(previously known as thyroid microsome autoantibodies) are present at:
high titre, in:
- Hashimoto's thyroiditis
- idiopathic thyroid atrophy
low titre, in:
- Grave's disease
- De Quervain's thyroiditis
- Without thyroid disease in 8% of males, and 10% of females
High titres of thyroid autoantibodies, particularly to thyroid microsomes,
is associated with increased likelihood of progress to myxoedema
as it reflects increased damage to the thyroid cells.
Other thyroid autoantibodies are not routinely measured.
TRH test
The TRH stimulation test has largely been replaced by highly sensitive TSH assays.
BUT STILL....
The administration of TRH injection 200 mcg IV
After 20 minutes produces a rise in serum TSH
This test is indicated to exclude hyperthyroidism in borderline cases
or where measures of serum T4 and T3 are equivocal:
A rise in TSH to outside the normal basal range excludes hyperthyroidism
i.e tsh is not being suppressed
An absent or impaired TSH response is consistent with
- Hyperthyroidism
- Grave's ophthalmology
- Some euthyroid multinodular goitres
- Subclinical toxic adenoma
- De Quervain's thyroiditis
- Acromegaly
- Hypopituitarism
- Cushing's disease
- TSH may also be impaired if too much thyroxine is given to hypothyroid patients
-